The Science of Pain: What It Is, How It Works, and How It's Managed
Pain is your body’s built-in alarm system. It’s how your brain alerts you that something might be wrong — whether it’s a stubbed toe, a pulled muscle, or damage to a nerve. But not all pain is created equal, and understanding the different types of pain can help explain why some treatments work better than others.
Types of Pain
Acute Pain
This is the kind of pain you feel when something suddenly hurts — like touching a hot stove or spraining your ankle. It’s usually sharp, has a clear cause, and goes away once the injury heals.
Chronic Pain
Pain that lasts longer than a few months is called chronic pain. It can come from ongoing conditions like arthritis, old injuries, or problems in the nerves or spine.
Neuropathic Pain
This type of pain comes from damage or dysfunction in the nervous system itself — the nerves, spinal cord, or brain. It can feel like burning, tingling, stabbing, or shooting sensations, and it doesn’t always go away when the injury heals. Think of it like a faulty wiring system sending out the wrong signals.
Centralized Pain
In some cases, the brain itself becomes more sensitive to pain signals. The volume gets turned up, even if the injury is minor or has healed. This is seen in conditions like fibromyalgia.

According to the International Association for the Study of Pain, pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage."
The Impact of Pain
Pain is the number one reason patients present to physicians. 19% of adults in the United States report persistent pain (defined as constant or frequent pain lasting for at least 3 months).
In a 2014 study by Kennedy et al, rates of persistent pain were highest for
Women
Adults ages 60–69 years
Adults who rated their health as fair to poor
Adults who were overweight or obese
Adults who were hospitalized one or more times in the preceding year.
Patients with chronic pain utilize about twice as many health care resources as the general population. In 2010, U.S. health care costs secondary to pain ranged from $560 billion to $635 billion (Gaskin and Richard 2012).
Pain Signals: The Basics
Your body is full of sensors — like alarm buttons — that detect things like pressure, temperature, and injury. These sensors send signals through nerves to your spinal cord and up to your brain, which interprets the signals as pain. But the brain isn’t just a passive observer — it can amplify or dampen pain based on factors like stress, mood, past experiences, and even expectations.
This is why two people with the same injury can feel very different levels of pain.
Nociceptors
Pains signals are detected by sensory neurons called nociceptors. Nociceptors, also called pain fibers, are neurons that detect damage to tissues and then transmit pain signals to the spinal cord. Different nociceptors detect different types of painful stimuli.
Nociceptors may be myelinated (axons are insulated by a myelin sheath) or unmyelinated (no myelin sheath around the axon). Myelination increases the conduction velocity, or speed, of signals (i.e., action potentials) as they travel to their destination.
The different types of nociceptors (i.e., pain fibers) are illustrated below.
A-delta Types I and II (myelinated) fibers rapidly transmit signals for "sharp" pain to the spinal cord.
C fibers (unmyelinated) fibers slowly transmit signals for "dull" pain to the spinal cord. C fibers have been implicated in chronic pain.
Nociceptors have free nerve endings (unlike receptors for touch/vibration which have corpuscles) and respond to a range of physical and chemical stimuli.
Normally, nociceptors only respond to signals capable of causing damage. If these receptors become hypersensitive, pain signals can be transmitted even in the absence of tissue damage.
A-Beta Fibers
Another type of sensory neuron, called A-Beta fibers, transmit non-noxious mechanical stimuli such as light touch, pressure, and vibration signals to the spinal cord. These fibers are myelinated, so the signal travels fast.
Sharp and Dull Pain
Have you ever stubbed your toe? Immediately after stubbing your toe, your reflexes kick in and you immediately withdraw your foot. The immediate pain you feel is from the A-delta fibers. Within milliseconds, the dull pain sets in and you REALLY feel it. The delay occurs because C-fibers travel slower than the A-delta fibers.
See the diagram below, which illustrates the fast and slow responses of A-delta and C fibers, respectively.
How Pain Signals Travel to the Brain
After an injury, immune cells and damaged tissue release chemicals such as bradykinin, prostaglandin, potassium, substance P, and histamine which activate nociceptors. Nociceptors send pain signals to the spinal cord (specifically, the dorsal horn of the spinal cord).
Once the pain signals reach the dorsal horn of the spinal cord, the signals are altered and modified by other neurons. These other neurons originate from various areas and modify pain signals. Serotonin neurons, norepinephrine neurons, or opioid-producing neurons are all involved in dampening or decreasing the intensity of the pain signals in the spinal cord before they travel up to the brain. This is why serotonin and norepinephrine medications like duloxetine (Cymbalta) and nortriptyline (Pamelor) are helpful for pain management.
Why We Rub Our Wounds
In addition to nociceptors, there are also nerve fibers called mechanoreceptors that originate outside the spinal cord and carry non-painful mechanical signals such as vibration, soft touch, and pressure from your muscles and skin. These mechanoreceptors also synapse on neurons in the dorsal horn of the spinal cord where they decrease or dampen pain signals. This is why we rub our wounds!
Opioid-Producing Neurons
As we've discussed, there are a number of neurons (e.g., mechanoreceptors, serotonin neurons, and norepinephrine neurons) that diminish pain signals in the spinal cord. Opioid-producing neurons are another type of neuron that diminish pain signals. Endogenous opioids are opioids produced naturally by our bodies. They play a role in dampening the pain signals in the dorsal horn of the spinal cord. This is why we use opioid medications (e.g., hydrocodone, morphine, fentanyl) for pain management.
How We Perceive Pain
Pain is not just something that happens in your body — it’s something your brain creates in response to signals it receives. Your brain doesn’t just passively receive those signals — it interprets them.

That interpretation is shaped by many factors: your emotions, past experiences, attention, expectations, and even your beliefs. For example, if you're anxious, stressed, or anticipating pain, your brain might amplify the signal. On the other hand, distraction, calmness, or reassurance can actually dampen the pain response.
In other words, pain is not just in your body — it’s in your mind and brain, too. That doesn’t make it “all in your head,” but it does mean that perception plays a powerful role in how pain is felt and how it can be treated.
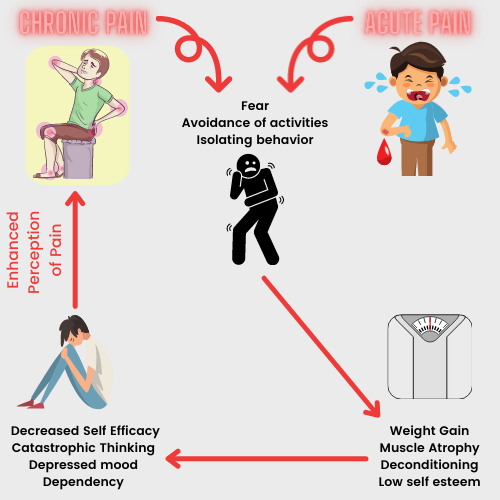
The Vicious Cycle of Chronic Pain
When pain becomes persistent, it’s natural to start avoiding activities that might make it worse. But over time, this avoidance can actually make the pain worse.
Here’s how the cycle works:
Pain leads to avoidance of movement or activity.
Avoidance causes muscle weakness, stiffness, and deconditioning.
These physical changes make movement harder and more painful.
This increases fear and further avoidance, which can also lead to isolation, anxiety, or depression.
The result is more pain, less function, and feeling stuck.
Breaking this cycle often means gently reintroducing movement, building confidence, and addressing the emotional side of pain — not just the physical symptoms.
The Treatment of Pain
Treating pain often means targeting different parts of this alarm system — the sensors, the nerves, the spinal cord, and the brain. Treatments are typically grouped into a few major categories:
(1) Medications
Anti-inflammatories (Nonsteroidal Anti-inflammatory Drugs/NSAIDs like ibuprofen or Steroids like prednisone): Block chemicals that cause inflammation and swelling.
Muscle relaxants (like tizanidine, cyclobenzaprine, methocarbamol, or baclofen): Help reduce muscle tension that can worsen pain.
Anticonvulsants and Nerve-stabilizing drugs (gabapentin, pregabalin, Carbamazepine, Oxcarbazepine): Calm overactive nerves in conditions like sciatica or diabetic neuropathy.
Antidepressants (like duloxetine, nortriptyline, or amitriptyline): Help regulate pain processing in the brain and spinal cord.
Topicals (like lidocaine patches, Capsaicin creams): Numb localized areas of pain.
NMDA Antagonists (Dextromethorphan, Memantine, Ketamine): Off label, but has mechanistic plausibility and anecdotal evidence.
Opioids: Powerful pain relievers that affect how the brain perceives pain — but they come with serious risks and are not ideal for long-term use.
Short-Acting Opioids (Immediate Relief): Hydrocodone (e.g., Norco, Vicodin – combined with acetaminophen), Oxycodone (e.g., Percocet – with acetaminophen; also available as plain oxycodone), Morphine (e.g., MSIR – morphine sulfate immediate release), Hydromorphone (e.g., Dilaudid), Codeine (often combined with acetaminophen; less potent), Tramadol (e.g., Ultram – weaker opioid with Serotonin-Norepinephrine Reuptake Inhibition properties)
-
Long-Acting Opioids (Extended Pain Control): Oxycodone ER (e.g., OxyContin), Morphine ER (e.g., MS Contin, Kadian, Avinza),
Hydromorphone ER (e.g., Exalgo), Fentanyl patches (e.g., Duragesic – transdermal, changed every 72 hours), Methadone (used for chronic pain and opioid use disorder, complex pharmacokinetics), Buprenorphine (e.g., Butrans patch, Belbuca film – partial agonist used for pain and opioid use disorder)
Supplements: Alpha-lipoic acid, Acetyl-L-carnitine, Omega-3 fatty acids, magnesium, Cannabidiol (CBD)
(2) Physical Therapy and Chiropractic Interventions
Movement, stretching, strengthening, and posture work can reduce pain over time — especially for back, joint, and nerve-related pain. Chiropractic adjustments can also be very helpful.
(3) Interventional Procedures
Surgical interventions, Nerve blocks, spinal injections, and devices like spinal cord stimulators can be used to interrupt pain signals when medications aren’t enough.
(4) Mind-Body Approaches
The brain plays a central role in how we experience pain, so treatments like:
Cognitive behavioral therapy (CBT)
Mindfulness meditation
Biofeedback
Massage
Acupuncture
can help people manage pain by reducing stress, improving sleep, and changing how the brain responds to pain.
There’s no one-size-fits-all approach to pain. What works for one person might not work for another — especially with chronic or neuropathic pain. The goal is to find the right combination of treatments that reduce pain, improve function, and help you live a fuller life.
References
Arciniegas, Yudisorderfsky, Hales (editors). The American Psychiatric Association Publishing Textbook Of Neuropsychiatry And Clinical Neurosciences. Sixth Edition.
Bear, Mark F.,, Barry W. Connors, and Michael A. Paradiso. Neuroscience: Exploring the Brain. Fourth edition. Philadelphia: Wolters Kluwer, 2016.
Higgins, E. S., & George, M. S. (2019). The neuroscience of clinical psychiatry: the pathophysiology of behavior and mental illness. Philadelphia: Wolters Kluwer.
Levenson, J. L. (2019). The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. Washington, D.C.: American Psychiatric Association Publishing.
Neuroscience, Sixth Edition. Dale Purves, George J. Augustine, David Fitzpatrick, William C. Hall, Anthony-Samuel LaMantia, Richard D. Mooney, Michael L. Platt, and Leonard E. White. Oxford University Press. 2018.
Stahl, S. M. (2013). Stahl's essential psychopharmacology: Neuroscientific basis and practical applications (4th ed.). New York, NY, US: Cambridge University Press.
Stern, T. A., Freudenreich, O., Fricchione, G., Rosenbaum, J. F., & Smith, F. A. (2018). Massachusetts General Hospital handbook of general hospital psychiatry. Edinburgh: Elsevier.
Whalen, K., Finkel, R., & Panavelil, T. A. (2015). Lippincotts illustrated reviews: pharmacology. Philadelphia, PA: Wolters Kluwer.
Hales et al. The American Psychiatric Association Publishing Textbook of Psychiatry. 6th Ed.
This post has been reviewed by a licensed medical professional.
.png)
.png)


.png)