Obsessive Compulsive Disorder
Being a "neat freak" has little to do with obsessive compulsive disorder. Obsessive Compulsive Disorder (OCD) is a type of anxiety disorder where individuals experience intrusive and unwanted thoughts (or images) followed by compulsive behaviors that attempt to reduce the anxiety and distress.
What are Obsessions?
Obsessions are intrusive thoughts (or images, feelings, or sensations) that pop up at inconvenient times and stay there. These awful thoughts can cause a lot of anxiety and distress. This is because those suffering with OCD attach greater meaning and significance to every thought, feeling, or experience they have.
The figure below illustrates this point. The marbles represent all the thoughts, feelings, and sensations we have, and the spotlight represents the focus of our attention.

Normally, we filter the thoughts, feelings, and sensations we experience and only direct our attention to those that are truly meaningful and important. However, those with obsessive compulsive disorder (and other anxiety disorders) place significance on nearly every thought, emotion, and sensation they experience. This is because the "alarm system" is constantly signaling that "something is wrong."
It's difficult to be mentally present when our attention is constantly being hijacked and directed to the thoughts, feelings, and sensations that we believe are significant. It's also an exhausting existence.
Obsessions are usually mental events.
A few examples of obsessions include
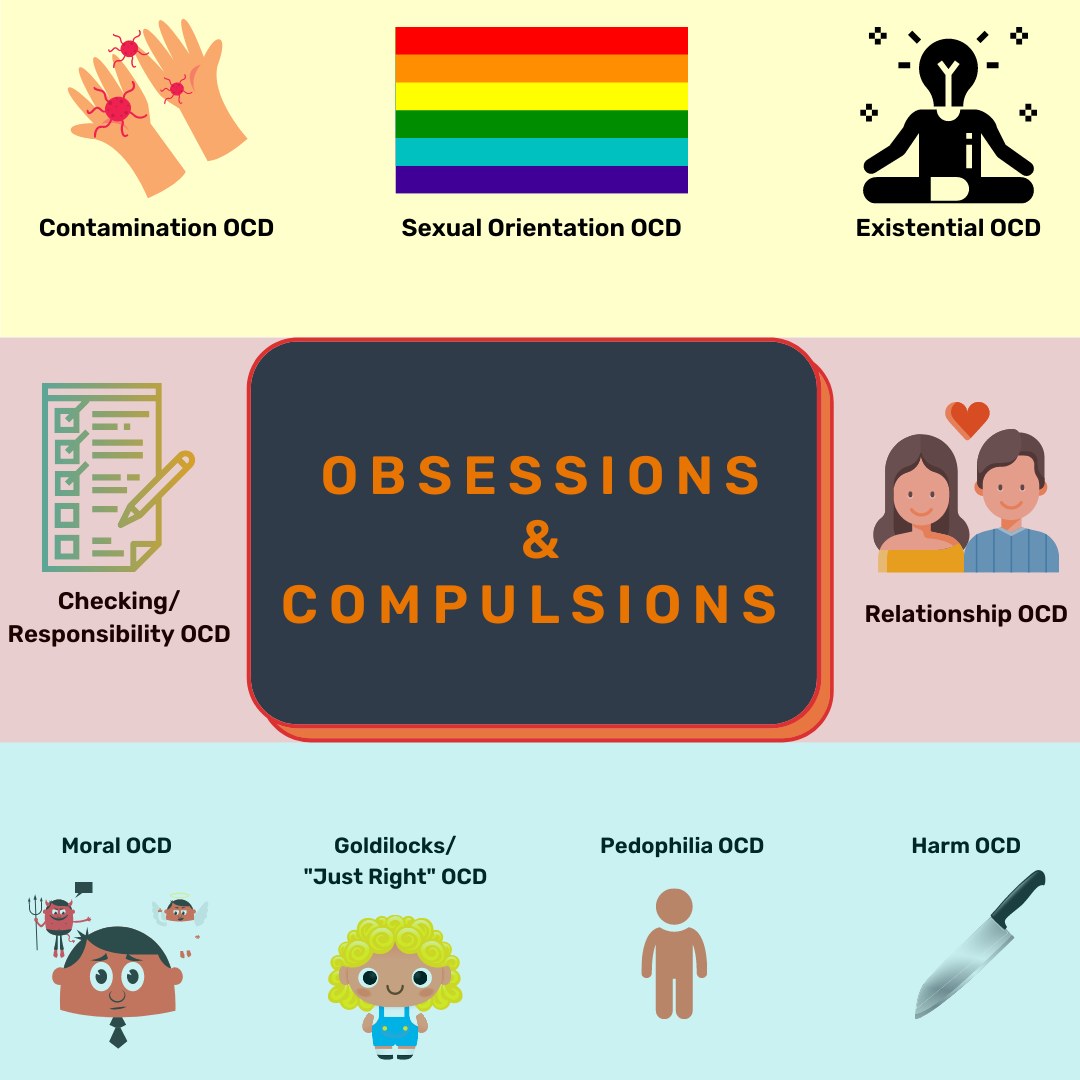
Contamination fears (fears about being contaminated with germs or being dirty)
Health obsessions (worrying about having cancer or some other devastating disease without any clinical evidence that it exists)
Responsibility obsessions
Harm obsessions (e.g., fear of losing control and hurting self or others)
Sexual orientation obsessions (e.g., fear of being homosexual)
Pedophilia Obsessions (e.g., worrying about being a pedophile)
Perfectionism or "just right" obsessions
Moral or religious obsessions (e.g., worrying about being an immoral or horrible person)
Relationship obsessions (e.g., doubt about love, doubt about your attraction to your partner, obsessing about being with the wrong partner)
Existential obsessions (e.g., meaning of life, "right" way of living)
What are compulsions?
In an attempt to reduce distress and anxiety from obsessions, individuals with OCD may perform compulsive rituals that are repetitive and time-consuming. These repetitive acts are called compulsions. By definition, a compulsion is a conscious, standardized, recurrent behavior, such as counting, checking, or avoiding. Compulsions may be mental or behavioral events. Compulsive acts are carried out in an attempt to relieve the anxiety associated with the obsession. Resisting a compulsive act increases anxiety.
A few examples of compulsions include
Washing hands or body repeatedly/Showering
Repeating compulsions ("saying a word, phrase, body movement)
Difficulty letting items go (i.e., hoarding)
Cutting, burning, banging, hitting, picking
Checking
Counting
Thought Neutralization (e.g., attempting to "undo" a thought)
Mental checking
Memory hoarding
Mental Review (ruminating)
Mental rehearsal
Analyzing hypothetical scenarios
Rationalizing
Overcontrol compulsions
Symmetry/Exactness/Evening Up compulsions (e.g., "just right")
Self-punishment and self-criticism
Compulsive Prayer
Compulsive Flooding
Compulsive reassurance seeking (e.g., researching online, visiting medical providers repeatedly, asking others if certain thoughts, feelings, sensations are "normal," comparing self to others as a barometer for "living the right way")
Avoidance
These compulsive behaviors can be time-consuming, unproductive, and even harmful. To the person experiencing them, they are torturous and stressful.
Because these behaviors are irrational and stressful to the individual experiencing them, they are called ego dystonic. This is in contrast to individuals with Obsessive Compulsive Personality who are perfectionists not distressed by their thoughts and behaviors because they align with their values and beliefs (i.e., ego syntonic).
A Disorder of Pathological Doubt
OCD and related disorders (e.g., eating disorders, hair pulling, skin picking, drug use, hoarding, phobias) can be thought of as disorders of doubt.
That is, persistent feelings of doubt and yearning for reassurance are prominent features of OCD and related disorders. One of the most debilitating aspects of these disorders is the insatiable nature of the compulsive behavior that never quite reaches an acceptable level of reassurance. This leads to tortuous repetition of the compulsive acts/reassurance-seeking behaviors despite the individual recognizing their irrational nature (ego dystonic).

There are numerous symptom "themes" or "types" of OCD, and many have more than one "theme" of OCD. Note that the diagram below is NOT an all-inclusive list.
Epidemiology
OCD is the 4th most common outpatient psychiatric diagnosis with approximately 10% of people having the diagnosis in psychiatric clinics. Epidemiological studies in Europe, Asia, and Africa have confirmed these rates across cultural boundaries. Females are slightly more affected than males in adulthood whereas boys are 2-3 times more affected than girls in childhood. Mean age of onset is approximately 19.5 years old. Males typically have an earlier age of onset than females. It is important to note that OCD rarely develops after age 35.
Risk Factors
Risk factors for developing OCD include genetic factors and environmental factors (e.g., psychosocial stressors, developmental problems, trauma, abuse, perinatal complications, infections). There is ongoing controversy around the purported association of childhood streptococcal infections and risk of developing obsessive compulsive disorder. Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infections (PANDAS) is a controversial autoimmune disorder believed to develop in children after group A beta hemolytic streptococcal infections. Antibodies to GABHS also attack health brain regions causing acute and rapid onset of tics and other OCD symptoms.
Associated Conditions
About 90% of patients with OCD suffer from other disorders such as anxiety disorders, depression, bipolar disorder, impulse control disorders, substance use disorders, and Tourette's disorder (i.e., tic disorders). Up to 50% of children suffering with OCD also suffer from attention deficit hyperactivity disorder, separation anxiety disorder, specific phobias, generalized anxiety disorder, and Tourette's disorder (i.e., tic disorders).
Other Disorders related to OCD
Body Dysmorphic Disorder (BDD)
Body Dysmorphic Disorder is a type of OCD-related disorder whereby individuals are preoccupied with an imagined defect in appearance which causes clinically significant distress. If a slight physical anomaly is actually present, the individual's concern with the anomaly is excessive and bothersome. BDD is often accompanied by compulsions such as Mirror checking, Excessive grooming, and Comparing appearance to others. Women are more commonly affected than men and the age of onset is typically between 15 years old and 30 years old. Individuals with BDD often suffer with mood disorders, anxiety disorders, and psychotic disorders. Individuals with BDD are more commonly seen in Plastic Surgery Clinics, Dermatology Clinics, and/or Primary Care Clinics.
Hoarding Disorder
Hoarding Disorder is another type of OCD-related disorder whereby individuals acquire and "hoard" unimportant possessions with little or no value due to an obsessive fear that may be needed in the future. This is a disorder of distorted beliefs about the importance of possessions. There is often excessive emotional attachment to possessions. The hoarding behavior leads to Cluttering, Unsanitary living conditions, Health risks (falls, animal born diseases), and Fire risks. Hoarding Disorder is commonly diagnosed in single persons with social anxiety or dependent personality traits. However, Hoarding Disorder can occur as a manifestation of other disorders/diseases such as dementia, Cerebrovascular disease, and schizophrenia. Unfortunately, most individuals with Hoarding Disorder not present to mental health clinics because most lack insight into their illness (ego-syntonic).
Hair-Pulling Disorder (Trichotillomania)
Trichotillomania was coined by a French dermatologist Francois Hallopeau in 1889 and is a chronic disorder characterized by repetitive hair pulling which results in hair loss. There is increased tension prior to hair pulling and relief of tension or gratification after the hair pulling. Women are affected more than men (10:1). Roughly 35%-40% of individuals with Trichotillomania chew or swallow their hair. Swallowing hair increases the risk of Bezoars (hairballs in the GI tract) which can cause obstruction.
Excoriation (Skin-Picking) Disorder
Compulsive and repetitive picking of the skin. 1-5% lifetime prevalence. Women are affected more than Men. It is important to rule out stimulant-induced excoriation. Skin picking is most often seen on the Face but also Legs, Arms, Torso, Hands, Cuticles, Fingers, Scalp. Embarrassment leads to avoidance and social withdrawal. 12% of skin-picking patients have attempted suicide.
Olfactory Reference Syndrome
A false belief by the patient that he or she has a foul body odor. The odor is not perceived by others. Leads to excessive showering, changing clothes. May rise to level of somatic delusion (Delusional Disorder). It is important to rule out "organic" illnesses such as Temporal lobe epilepsy, Pituitary tumors, and Sinusitis. Currently there is little evidence for treatment.
Medication or Drug-Induced Obsessive-Compulsive Symptoms
The following medications/drugs have been associated with worsening or causing obsessive compulsive symptoms:
Psychostimulants
Amphetamines
Methylphenidate (rare)
Methamphetamine
Cocaine
Nicotine
MDMA (Ecstasy)
PCP
Synthetic Cathinones ("Bath Salts")
Dopamine agonists
L-dopa
Ropinirole
Pramipexole
Aripiprazole (Abilify)
Bromocriptine
Amantadine
Bupropion
Medical Problems associate with OCD Symptoms
The following medical problems/neurological disorders have been associated with obsessive compulsive symptoms as part of the natural course of the illness:
Huntington's Disease
Wilson's Disease
Seizures
Surgery-Related
Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infections (PANDAS)
Treatment Options
Current evidence suggests that medication (e.g., selective serotonin reuptake inhibitors) and/or exposure response prevention therapy are the most effective approaches to managing symptoms of OCD. By becoming consciously aware of the doubt cycle and its chain of events, one learns how to respond differently--starting with regaining cognitive and emotional balance through the application of acceptance strategies and mindfulness-based practices.

Problems with Treatment
20-30% of patients have significant improvement in symptoms with medication alone (this is increased when combined with therapy). 40-50% of patients have moderate improvement. Higher doses of SSRIs may be required to alleviate symptoms in OCD compared to depression. Higher doses of SSRIs means greater likelihood for developing side effects from these medications.
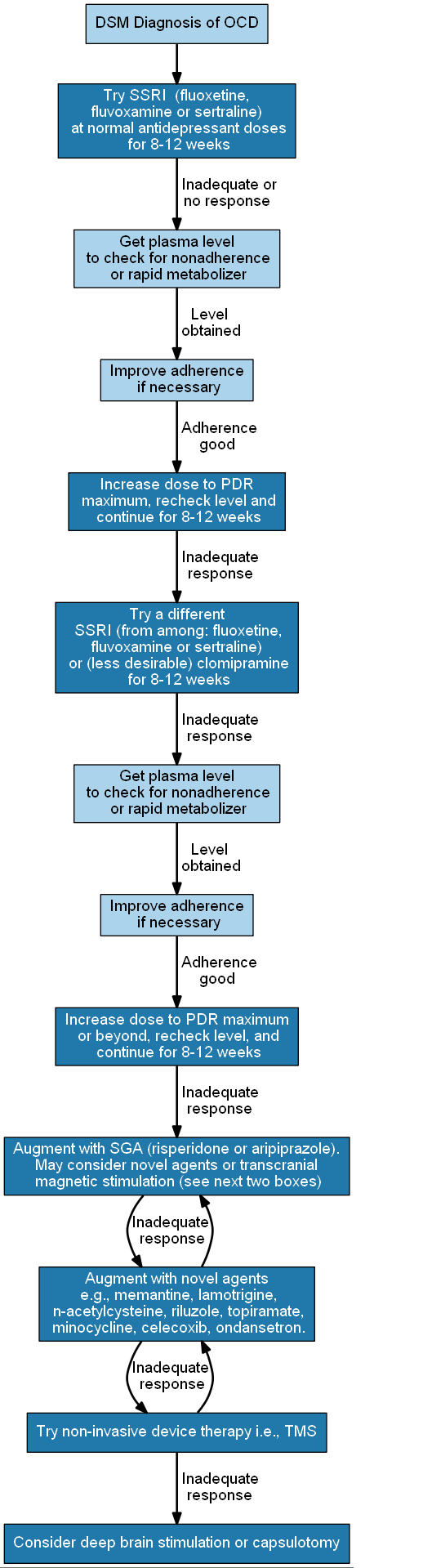
MEDICAL (MEDICATION) TREATMENT ALGORITHM FOR OBSESSIVE COMPULSIVE DISORDER
The algorithm below is from the Psychopharmacology Algorithms Project at the Harvard South Shore Psychiatry Residency Training Program led by David Osser, MD.
EXPOSURE RESPONSE PREVENTION THERAPY (ERP)
Exposure Response Prevention Therapy remains the most effective therapeutic modality for OCD and related disorders.
Exposure and response prevention (ERP) is a form of cognitive behavioral therapy (CBT) used to treat a variety of conditions, including anxiety, phobias, and eating disorders. It is considered the gold-standard treatment for obsessive-compulsive disorder (OCD).
As stated previously, OCD and related disorders can be thought of as disorders of pathological doubt—the persistent feeling of doubt and the need for reassurance are prominent features.
One of the most debilitating aspects of OCD is the insatiable nature of the compulsive behavior that never quite reaches an acceptable level of reassurance. This leads to tortuous repetition of the compulsive acts/reassurance-seeking behaviors.
Exposure and response prevention is designed to gradually reduce the anxiety that feeds obsessions and compulsions.
One way in which this is thought to happen is through a process called habituation, whereby we become less physiologically aroused by triggering stimuli or obsessions after being repeatedly and safely exposed to them.
Individuals with OCD, anxiety, phobias, or eating disorders learn that the stimuli, thoughts, and feelings that prompt compulsions are more bearable than anticipated.
You will also realize that being exposed to your fears does not actually lead to the outcomes you dread. Over time, you will come to recognize that you’re capable of coping with the triggers without resorting to compulsive rituals.
How Does Exposure Response Prevention (ERP) Work?
Exposure and response prevention involves two steps:
EXPOSURE: Directly exposing yourself to thoughts or situations that generally evoke fear, distress, obsessive thoughts, or compulsive, ritualistic behavior.
RESPONSE PREVENTION: Use deep breathing, distractions, and other techniques to prevent the usual reassurance-seeking response. Over time, you will get accustomed to experiencing a trigger but not giving in to the compulsion.
The greatest challenge of ERP is the “response prevention” part—learning not to respond to the obsessions with the usual compulsive behaviors.
With exposure to increasingly uncomfortable stimuli, you will learn to tolerate the distress without having to resort to rituals which only perpetuate the cycle.

ERP is about facing your fears and learning that it isn't that bad (even though it feels bad in the moment).
References
Afshar, Hamid et al. "N-Acetylcysteine Add-On Treatment in Refractory Obsessive-Compulsive Disorder." Journal of Clinical Psychopharmacology (2012): 797-803. Print.
Pauls, David L., Amitai Abramovitch, Scott L. Rauch, and Daniel A. Geller. "Obsessive–compulsive Disorder: An Integrative Genetic and Neurobiological Perspective." Nature Reviews Neuroscience Nat Rev Neurosci (2014): 410-24. Print.
Oliver, Georgina, Olivia Dean, David Camfield, Scott Blair-West, Chee Ng, Michael Berk, and Jerome Sarris. "N-Acetyl Cysteine in the Treatment of Obsessive Compulsive and Related Disorders: A Systematic Review." Clin Psychopharmacol Neurosci Clinical Psychopharmacology and Neuroscience (2015): 12-24. Print.
"Obsessive Compulsive Disorder." Dynamed.
Sadock, Benjamin J., and Harold I. Kaplan. Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/clinical Psychiatry. 10th ed. Philadelphia: Wolter Kluwer/Lippincott Williams & Wilkins, 2007. Print.
Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association, 2013. Print.
Stahl’s Essential Psychopharmacology, 4th Edition. Cambridge University Press. 2013
Iversen, L. L., Iversen, S. D., Bloom, F. E., & Roth, R. H. (2009). Introduction to neuropsychopharmacology. Oxford: Oxford University Press.
Levenson, J. L. (2019). The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. Washington, D.C.: American Psychiatric Association Publishing.
Mendez, M. F., Clark, D. L., Boutros, N. N. (2018). The Brain and Behavior: An Introduction to Behavioral Neuroanatomy. United States: Cambridge University Press.
Schatzberg, A. F., & DeBattista, C. (2015). Manual of clinical psychopharmacology. Washington, DC: American Psychiatric Publishing.
Schatzberg, A. F., & Nemeroff, C. B. (2017). The American Psychiatric Association Publishing textbook of psychopharmacology. Arlington, VA: American Psychiatric Association Publishing.
Sixth Edition. Edited by Dale Purves, George J. Augustine, David Fitzpatrick, William C. Hall, Anthony-Samuel LaMantia, Richard D. Mooney, Michael L. Platt, and Leonard E. White.
Stern, T. A., Freudenreich, O., Fricchione, G., Rosenbaum, J. F., & Smith, F. A. (2018). Massachusetts General Hospital handbook of general hospital psychiatry. Edinburgh: Elsevier.
Hales et al. The American Psychiatric Association Publishing Textbook of Psychiatry. 6th Ed.
____
This post was reviewed by a medical professional.