Polypharmacy and Medication Interactions
Polypharmacy refers to the practice of administering or using multiple medications simultaneously to treat one or more health conditions. This approach is often used in the treatment of complex or multiple chronic diseases, where different drugs are necessary to manage different aspects of a patient's health. This practice is relatively common in clinical psychiatry.
Types of polypharmacy
Same‑Class Polypharmacy refers to the use of more than one medication from the same class (e.g., use of two selective serotonin reuptake inhibitors in a case of depression).
Multi‑Class Polypharmacy is the use of full therapeutic doses of more than one medication from different classes for the same symptom cluster (e.g., use of valproate along with an atypical antipsychotic, such as olanzapine, for treatment of mania).
Adjunctive Polypharmacy is the use of one medication to treat the side effects of another medication from a different class (e.g., using trazodone for insomnia caused by a stimulant).
Augmentation Polypharmacy refers to the use of one medication at a low dose along with another medication from a different class at a full therapeutic dose for the same symptom cluster (e.g., addition of low dose aripiprazole in a patient responding partially to a selective serotonin reuptake inhibitor); or the addition of a medication that would not be used alone for the same symptom cluster (e.g., augmentation of antidepressants with lithium or thyroid hormone).
Total Polypharmacy is the total count of medications used in a patient, or total drug load.
The efficacy of polypharmacy is difficult to assess given the dearth of clinical studies. Therefore, polypharmacy is mostly supported by clinical experience and case studies. And although the practice of combining two or more medications to relieve psychiatric symptoms can be beneficial, it also comes with elevated risks.
Benefits of Polypharmacy
Comprehensive Treatment: It allows for the treatment of multiple conditions at once, which can be crucial for patients with comorbidities.
Synergistic Effects: Some medications can work better together, offering a more effective treatment than either would alone.
Tailored Therapies: Polypharmacy can be used to fine-tune treatments for individual patients, taking into account their unique health profiles.
Risks of Polypharmacy
Adverse Drug Reactions: The more medications a person takes, the higher the risk of side effects and interactions between the drugs.
Medication Non-Adherence: Managing multiple medications can be complicated, leading to mistakes or non-adherence to treatment regimens.
Increased Healthcare Costs: Multiple medications mean higher costs, which can be a burden for patients and healthcare systems.
Geriatric Considerations: Older adults are particularly susceptible to the risks of polypharmacy due to physiological changes associated with aging and the increased likelihood of multiple chronic conditions.
Management of Polypharmacy
Managing polypharmacy effectively involves a balance between ensuring adequate treatment and minimizing potential risks. This includes regular review of the patient's medication regimen, considering the necessity of each medication, and monitoring for adverse effects or interactions. Education for patients and caregivers on proper medication management is also crucial.
Let's review the ways medications can interact to produce both positive and negative effects.

The most common types of drug-drug interactions
Medications can interact with each other in various ways, leading to either positive or negative effects. Understanding these interactions is crucial in healthcare, particularly in polypharmacy, where multiple drugs are prescribed.
Pharmacodynamic Interactions
Positive Effects: These occur when two drugs interact at their sites of action, potentially enhancing each other's effects. For instance, combining a Selective Serotonin Reuptake Inhibitor (SSRI) with a Dopamine-Norepinephrine Reuptake Inhibitor (DNRI) would theoretically target all three major monoamine neurotransmitter systems to alleviate a variety of depressive symptoms.
Negative Effects: Conversely, drugs can interact to cause excessive sedation, such as combining antihistaminergic medications (e.g., quetiapine, doxepin) with benzodiazepines, both of which depress the central nervous system.
Pharmacokinetic Interactions
Absorption: Medications can alter the absorption of others. For example, antacids can increase the absorption of amphetamines, increasing the potential for toxicity and side effects.
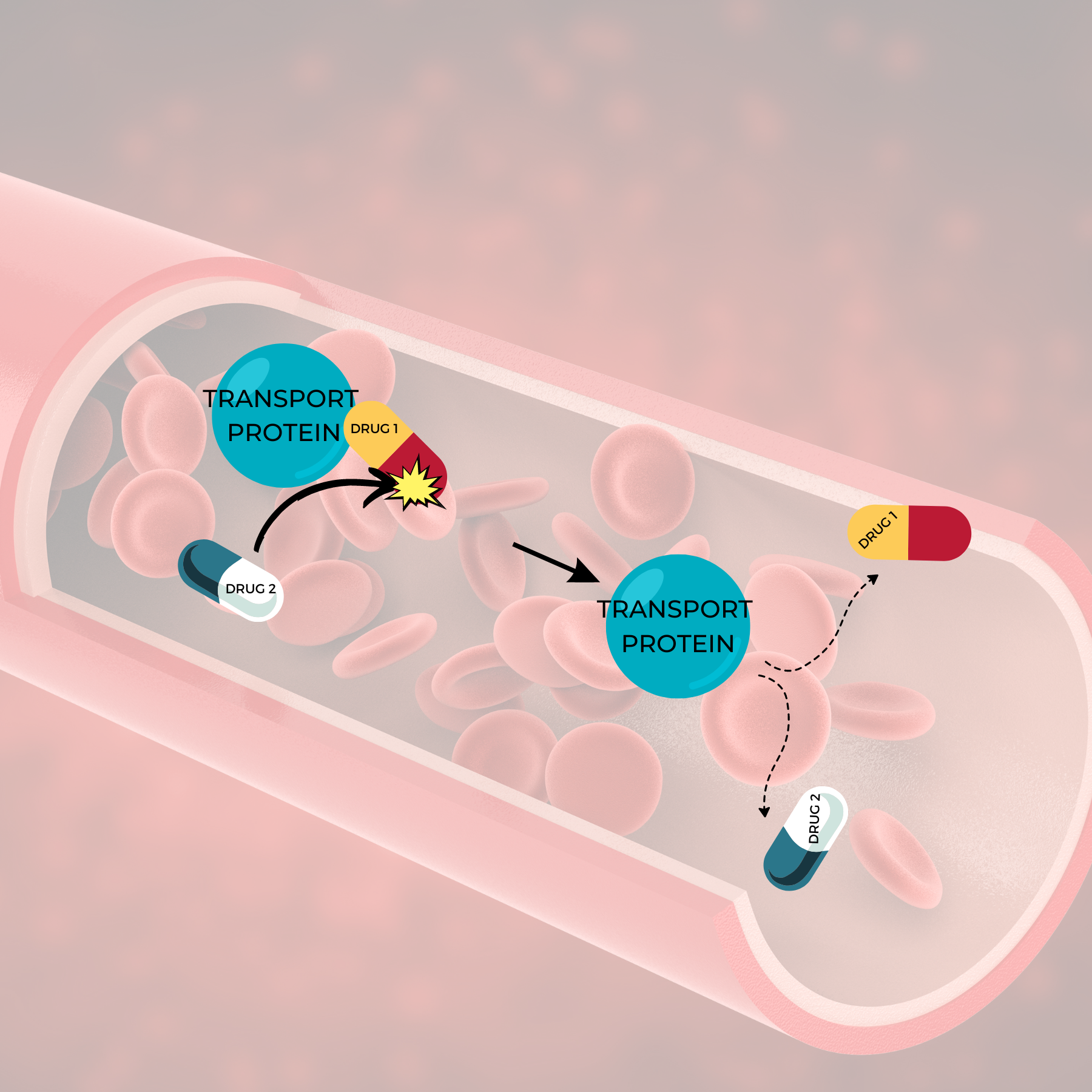
Distribution: Some drugs can compete for protein binding sites in the bloodstream, leading to increased levels of free drug, which can enhance or diminish effectiveness and increase the risk of side effects. That is, many medications travel in the bloodstream attached to proteins called "transport proteins." Some medications/drugs might remove or "kick off" a medication from its transport protein which would raise free drug concentrations in the blood.
Metabolism: Drugs can either induce or inhibit the enzymes responsible for metabolizing other drugs. Recall that enzymes are like "Pac-Man" that break down (or metabolize) drugs and medications. Some medications alter the activity of the enzymes that metabolize other medications and drugs. If an enzyme's activity is increased, then the medication metabolized by that enzyme may be metabolized or broken down too quickly. This results in decreased blood levels of the medication which may decrease the medication's effectiveness. If an enzyme's activity is decreased, then the medication metabolized by that enzyme may be metabolized or broken down too slowly. This results in increased blood levels of the medication which might cause side effects and toxicity.

Excretion: Some drugs can alter the body's ability to eliminate drugs and medications. This can occur when one drug alters the functioning of the kidneys, intestines, and/or liver, affecting the drug's elimination and therefore its concentration in the body.
Direct Chemical or Physical Interactions
These occur when drugs mix in a solution, potentially leading to inactivation of one or both drugs. For example, certain drugs precipitate when mixed together in an IV solution, rendering them ineffective.
Positive Interactions (Synergism)
Complementary Action: Different drugs can work together to enhance overall treatment effectiveness. For example, in cancer therapy, different drugs may target various pathways of tumor growth, leading to a more effective treatment.
Reduced Side Effects: Sometimes, one drug can help mitigate the side effects of another. For instance, anti-nausea medications are often given alongside chemotherapy to manage its side effects.
Negative Interactions
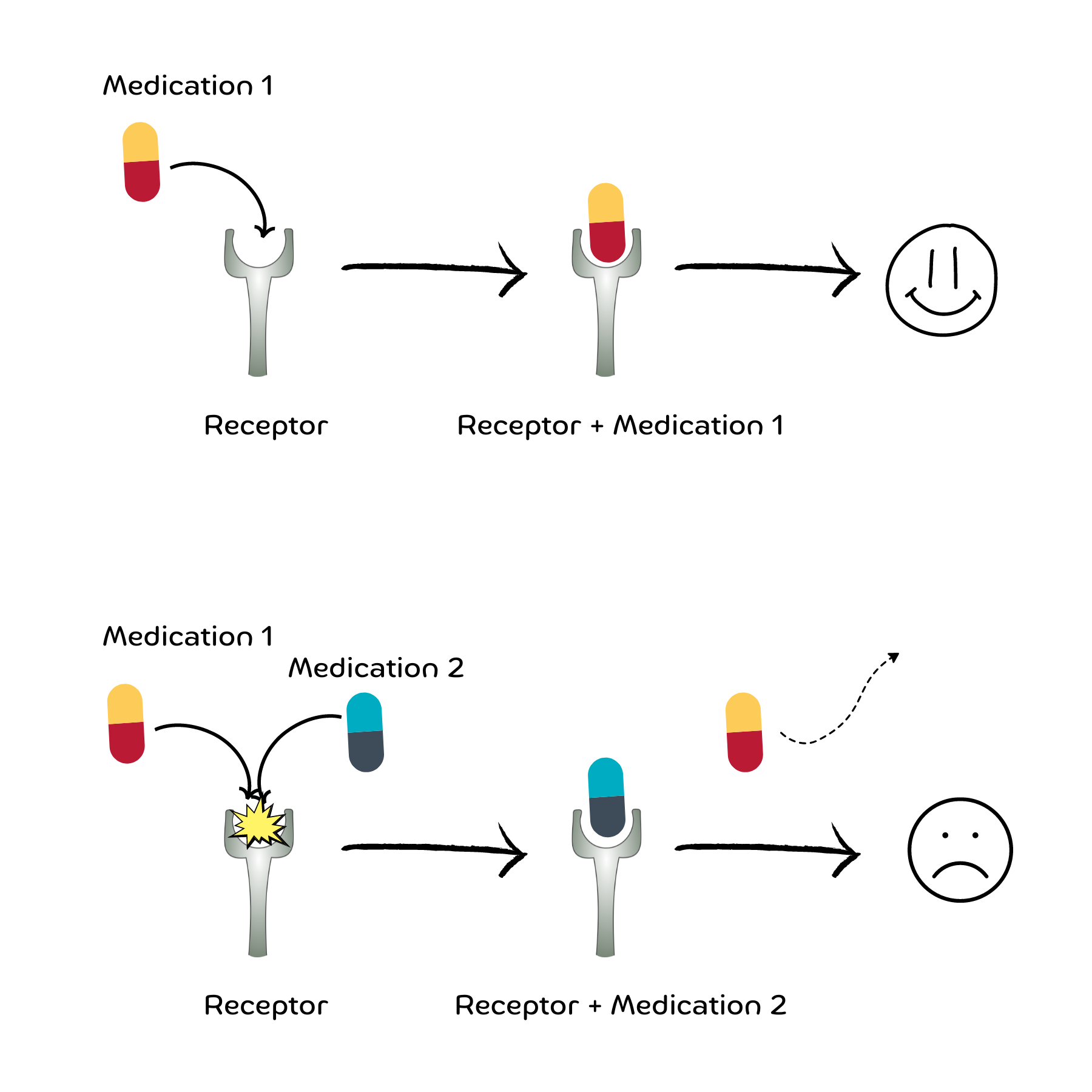
Antagonism: This occurs when one drug reduces or negates the effect of another. For instance, a drug or medication might compete with another drug or medication at the same receptor.
Increased Toxicity: Certain drug combinations can lead to increased toxicity. For example, combining two medications that are toxic to the liver can increase the risk of liver damage.
Below are the most common drug-drug interactions to be aware of when taking psychotropic medications (i.e., medications used to treat mental disorders)
Valproic acid (VPA, Depakote) + Lamotrigine (Lamictal)
Valproic acid (VPA) increases lamotrigine levels by decreasing lamotrigine metabolism
Increased lamotrigine levels increase the risk of developing a severe rash
Increased lamotrigine levels increase the risk of Steven-Johnson’s Syndrome (SJS/TEN)
When taking both valproic acid (Depakote) and lamotrigine (Lamictal), the general recommendation is to decrease the dose of lamotrigine by 50%
Carbamazepine (CBZ) is an inducer of CYP3A4
CBZ induces its own metabolism by increasing the activity of the CYP3A4 enzyme
CBZ also induces the metabolism of other medications that are metabolized by CYP3A4 such as oral contraceptives, clozapine, alprazolam, buspirone, and clonazepam
Lithium levels are INCREASED when combined with
Non-Steroid Anti-inflammatory Drugs (NSAIDs), except aspirin
Angiotensin Converting Enzyme Inhibitors (ACE Inhibitors)
Thiazide diuretics such as hydrochlorothiazide
Low sodium diets
Lithium levels are DECREASED when combined with
Caffeine
Theophylline
High sodium diets
Grapefruit Juice
Grapefruit juice is a potent inhibitor of CYP3A4 and P-glycoprotein (another protein that helps eliminate drugs)
Therefore, grapefruit juice increases blood levels of many medications metabolized by CYP3A4
Smoking Tobacco cigarettes
The hydrocarbons in the smoke of tobacco cigarettes, but not nicotine, increase the activity of CYP1A2 enzymes
Smoking cigarettes decreases blood levels of medications metabolized by CYP1A2 such as Olanzapine, Clozapine, and Caffeine
Tyramine + Monoamine Oxidase Inhibitors (MAOIs)
Tyramine (TIE-ruh-meen) is an amino acid that occurs naturally in the body and aids in regulating blood pressure. Elevated tyramine levels can lead to dangerously elevated blood pressures.
Tyramine is also found in certain foods such as banana peel, beer, fava beans, aged cheese, sauerkraut, sausage, soy sauce, and concentrated yeast extract.
An enzyme called monoamine oxidase (MAO) breaks down excess tyramine in the body. Monoamine oxidase inhibitors (MAOIs) are used to treat depression.
If taking a monoamine oxidase inhibitor, it is important to avoid certain foods high in tyramine.
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine oxidase (MAO) is an enzyme that breaks down monoamines such as serotonin, dopamine and norepinephrine. Therefore, monoamine oxidase inhibitors (MAOIs), such as selegiline and phenelzine, are used to treat depression.
Combining MAOIs with Selective Serotonin Reuptake Inhibitors (SSRIs), Tricyclic Antidepressants (TCAs), Pseudoephedrine, and Stimulants increases the risk of serotonin toxicity and dangerously high blood pressures
Fluoxetine, Paroxetine, and Bupropion are potent inhibitors of CYP2D6
Drugs like fluoxetine, paroxetine, and bupropion inhibit CYP2D6 enzymes and increase blood levels of other medications metabolized by CYP2D6.
Fluoxetine, paroxetine, and bupropion decrease the effectiveness of Tamoxifen and Codeine because Tamoxifen and Codeine require CYP2D6 activity to be effective.
Antimicrobial-Psychotropic Drug Interactions
Antimalarials increase levels of phenothiazines such as chlorpromazine (Thorazine)
Azoles increase levels of alprazolam, midazolam, and buspirone
Clarithromycin and Erythromycin increase levels of alprazolam, midazolam, carbamazepine, clozapine, and buspirone
Quinolones increase levels of clozapine and benzodiazepines (but decreases the effects of benzodiazepines)
Isoniazid increases levels of haloperidol and carbamazepine. Isoniazid + disulfiram can cause problems with motor coordination (called ataxia)
Isoniazid and Linezolid are weak inhibitors of monoamine oxidase (MAO) and therefore increases the risk of serotonin syndrome and hypertensive emergencies if used with serotonergic drugs (like SSRIs, SNRIs, and TCAs)
Erythromycin, Clarithromycin, and Ketoconazole + Tricyclic Antidepressants or antipsychotics
Combining Erythromycin, Clarithromycin, or Ketoconazole with Tricyclic Antidepressants or antipsychotics increases the risk of QT prolongation and cardiac (ventricular) arrythmias
Drug-Drug Interaction Tables




Conclusion
Understanding and managing medication interactions is a key aspect of psychopharmacological care. Healthcare providers must be vigilant about these interactions to optimize therapeutic outcomes and minimize risks for their patients.
___
This post was reviewed by a licensed medical professional.